Now what? UC Davis public health expert maps out COVID-19 status and road ahead
(SACRAMENTO) — COVID-19 cases and infection rates are skyrocketing. Gov. Gavin Newsom this week closed a range of California businesses - again. Local health officials warn about the explosive spread of the coronavirus – while we still see scenes of casual beach gatherings in places like South Lake Tahoe.
For many people, all the numbers and changing orders make it hard to get a solid picture of where we stand with COVID-19.
“There is a legitimate reason why they feel that way,” said Brad Pollock, chair of the UC Davis Health Department of Public Health Sciences. “Our situation continues to change, and not for the better.
“In many ways, we are worse off than we were three months ago,” Pollock said. “The increase we are seeing is real. Will we start to level off? I don’t know. I’m really concerned about that.”
Pollock is also the chair of the University of California’s Public Health COVID-19 Working Group. He’s been tracking the coronavirus for months and has an up-to-date overview of the Sacramento region and of California.
“We were doing well until Memorial Day weekend,” he said. “The coronavirus had been smoldering along. But pent-up energy around the holiday and the loosened restrictions gave people a false sense of security that COVID-19 was no longer a threat.”
An overview of the cases
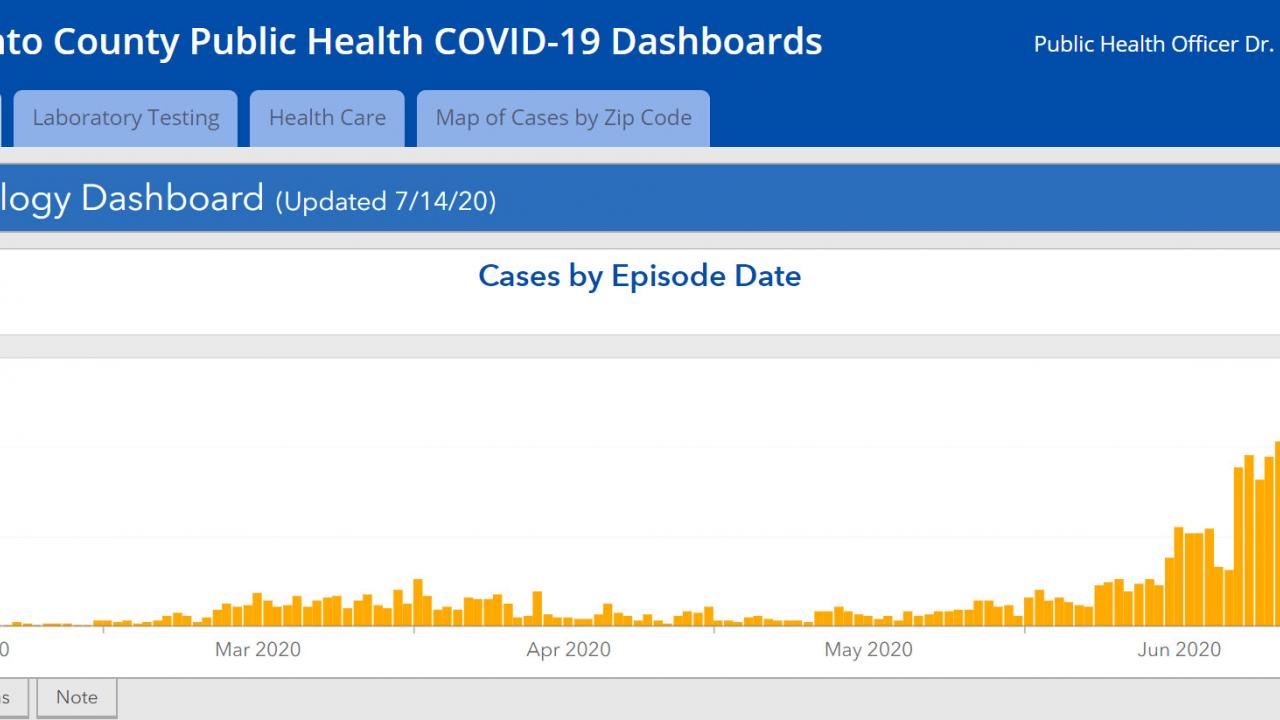
The numbers on the California and Sacramento County dashboards tell the story of the threat. Many other counties have similar trajectories:
- Cases have more than doubled in both Sacramento County and the state since June 1.
- It’s not because there is more testing. The percentage of tests coming back positive in Sacramento County was 6.7% in the first week of July. It was under 1% in late May.
- For all of California, the rate of positive tests in mid-July hit 8% vs. 4% in late May.
“What’s unnerving now is that we’re seeing the majority of cases are young people,” Pollock said. “They see themselves as low risk. It’s summer and they want to be out. They don’t see themselves as being personally vulnerable to the effects of COVID-19.”
Statewide, more than one-third of the infections are people aged 18 to 35. Expand that to 18-49 and that’s 60 percent of the infections in California and in Sacramento County. This data reflects similar percentages in other counties.
“What’s unnerving now is that we’re seeing the majority of cases are young people,” Pollock said. “They see themselves as low risk. It’s summer and they want to be out. They don’t see themselves as being personally vulnerable to the effects of COVID-19.”
Pollock said one of the public health goals is to get the message across that every person who is infected is likely to infect two to three other people on average.
“Many don’t understand that the people they will infect downstream may be their parents or their grandparents or their favorite aunt,” Pollock said.
Making health information resonate
He said one of the complications of getting public health information across is that knowledge about the coronavirus continues to evolve.
“This is science,” he said. “We started off knowing very little about the virus. Scientists all over the world are doing research, and what we know grows and changes. One of major issues of public health is that many people don’t take in nuances and they don’t want to change their minds.”
For instance, he said the research and information on masks has evolved and gotten clearer, but that message is meeting resistance for reasons ranging from stubbornness to politics.
“We now know face coverings are important in protecting each other and ourselves.” Pollock said. “We could get life restarted, but we need everyone to adhere to the public health recommendations. We need people to really hear that you can have your life, we just have to be responsible for each other. Seeing role models would help.”
Will the latest measures flatten the curve?
“There seems to have been some movement in behavior, maybe, and the latest restrictions will have an impact,” Pollock said. “We also know one of the major reasons COVID-19 has increased has been because of larger private gatherings. Those are harder to control.”
Public health leaders don’t have exact answers on the best ways to get people to follow health recommendations or do things like wear masks. Every situation is different. In March, for instance, Californians understood the need to shelter-in-place. Summer has seen much less caution, despite the soaring case numbers.
“Some people and business owners made up their minds it is OK to go back to their normal lives. Persuading them otherwise is complicated,” he said. “Sometimes you catch more flies with honey and with friendly reminders that you don’t help your business by getting your customers sick. But sometimes you have to go beyond honey, and that seems to be where we are now.”
So how effective will this round of warnings and re-imposed restrictions be?
“We’ll see in a couple weeks,” Pollock said.
What has improved: COVID-19 health care
“Early social distancing intervention made a huge difference in March,” Pollock said. “The idea was to bend the curve to prevent a surge that would overwhelm our hospitals and spike the death rate. People did such a good job of following the guidelines that within a few weeks, we saw the curve begin to shift.”
That flattened curve, particularly in the Sacramento region, allowed hospitals to establish protocols, plan for surges, stockpile supplies, learn best practices for treating COVID-19 patients and more.
“We are in far better shape to handle larger numbers of COVID-19 patients now,” Pollock said. “A lot of that is because we were not overrun in March and April.”
What happens next
“We are not going to reach herd immunity anytime soon, not without a vaccine,” Pollock said. “The coronavirus will likely smolder in our community for the next five or six months.”
Whether the number of cases, serious illness and deaths move up or down during that time will depend on whether most people follow recommended health guidelines.
“It’s very clear, if we can keep people physically separated by six feet or more, if they don’t gather indoors, if they wear masks, the chances of them picking up the virus are low,” he said. “That would translate into having some semblance of an opened-up economy.”
And does Pollock think most people will come around and, as he said, protect each other?
“I’m an optimist,” he said. “I still think if most people are armed with real information they can understand, they’ll do the right thing.”